The Rise of Smart Hospitals: Technology in Medical Facilities marks a pivotal shift in healthcare delivery. The integration of advanced technologies, from artificial intelligence and the Internet of Things (IoT) to robotics and telehealth, is revolutionizing patient care, operational efficiency, and the overall hospital experience. This transformation promises to enhance diagnostic accuracy, personalize treatment plans, improve patient safety, and ultimately, lead to better health outcomes.
This exploration delves into the advancements, impacts, challenges, and future trajectory of this rapidly evolving field.
This analysis examines the multifaceted impact of technological integration within medical facilities. We will explore the evolution of medical technology, the role of AI and machine learning in improving diagnostics and treatment, and the benefits of IoT devices in patient monitoring. Further, we will assess the influence of these advancements on patient care, examining aspects such as enhanced safety, improved access through telehealth, and the personalization of medical interventions.
The challenges and ethical considerations associated with data security, AI implementation, and cost-effectiveness will also be addressed, alongside a projection of future trends and the potential of emerging technologies like blockchain and virtual reality.
Technological Advancements in Smart Hospitals
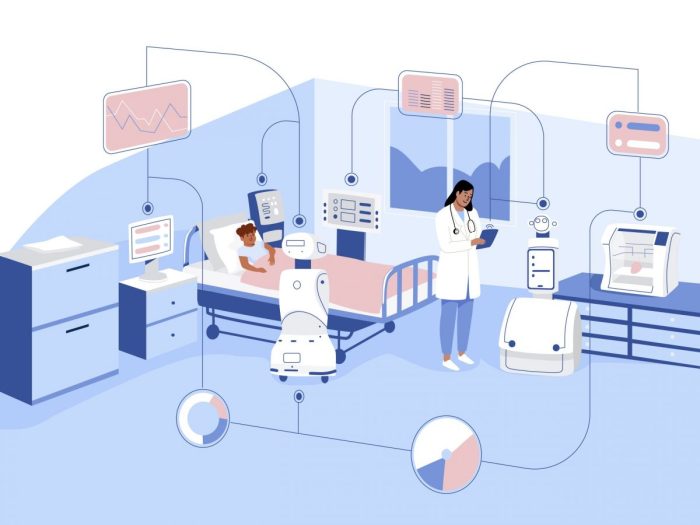
The evolution of medical technology has dramatically reshaped healthcare delivery, culminating in the rise of smart hospitals. These facilities leverage advanced technologies to enhance efficiency, improve patient outcomes, and optimize resource allocation. This transformation is driven by advancements in computing power, data analytics, and interconnected devices, leading to a more proactive, personalized, and data-driven approach to healthcare.
Evolution of Medical Technology Leading to Smart Hospitals
The journey towards smart hospitals began with the introduction of electronic health records (EHRs), replacing paper-based systems and enabling better data management and accessibility. This was followed by the integration of medical imaging technologies like MRI and CT scans, providing detailed diagnostic information. The development of minimally invasive surgical techniques and advanced medical devices further paved the way for more precise and efficient treatments.
The convergence of these advancements, coupled with the rise of artificial intelligence and the internet of things, has fueled the creation of truly “smart” hospitals.
Impact of AI and Machine Learning on Diagnosis and Treatment
Artificial intelligence (AI) and machine learning (ML) are revolutionizing diagnosis and treatment in smart hospitals. AI algorithms can analyze medical images (X-rays, CT scans, MRIs) with remarkable accuracy, detecting anomalies and assisting radiologists in making faster and more precise diagnoses. ML models can predict patient risk factors, personalize treatment plans, and optimize medication dosages, leading to improved patient outcomes and reduced hospital readmissions.
For example, AI-powered diagnostic tools are now being used to detect cancerous lesions earlier and more accurately than traditional methods. Similarly, ML algorithms are helping to predict the likelihood of patients developing sepsis, allowing for timely interventions.
Role of IoT Devices in Improving Patient Care and Monitoring
The Internet of Things (IoT) plays a crucial role in enhancing patient care and monitoring within smart hospitals. Wearable sensors, implanted devices, and connected medical equipment continuously collect patient data, such as heart rate, blood pressure, and oxygen saturation. This real-time data stream allows medical staff to proactively identify potential problems and intervene promptly. For example, remote patient monitoring using IoT devices enables early detection of deterioration in patients with chronic conditions, preventing hospital readmissions and improving quality of life.
Smart beds and infusion pumps can also be integrated into the IoT network, providing automated alerts and reducing medication errors.
Robotic Surgery and its Benefits
Robotic surgery is transforming surgical procedures, offering enhanced precision, minimally invasive approaches, and improved patient recovery times. Robotic surgical systems provide surgeons with a magnified, three-dimensional view of the surgical field, enabling greater dexterity and control. The smaller incisions associated with robotic surgery lead to reduced pain, scarring, and shorter hospital stays. Examples of robotic surgery applications include prostatectomies, hysterectomies, and cardiac procedures.
The da Vinci Surgical System is a widely used example of this technology, demonstrating the benefits of robotic assistance in complex surgical operations.
Comparison of Traditional and Smart Hospital Systems
| Area | Traditional System | Smart Hospital System | Key Improvements |
|---|---|---|---|
| Patient Monitoring | Manual checks, limited real-time data | Continuous monitoring via IoT devices, AI-driven alerts | Improved early detection of complications, proactive interventions |
| Diagnosis | Reliance on physical examinations and basic imaging | AI-powered image analysis, advanced diagnostics | Increased diagnostic accuracy, faster diagnosis times |
| Treatment | Standard treatment protocols, limited personalization | Personalized treatment plans based on AI and patient data | Improved treatment effectiveness, reduced side effects |
| Administration | Manual processes, paper-based records | Automated workflows, EHRs, data analytics | Increased efficiency, reduced administrative burden |
Impact on Patient Care and Experience

Smart hospital technologies are fundamentally reshaping patient care, improving safety, enhancing access, and personalizing treatment. The integration of various technological advancements leads to a more efficient, effective, and patient-centered healthcare system. This section will explore the significant impact of these technologies on the overall patient experience.
Enhanced Patient Safety and Error Reduction
The implementation of smart technologies significantly contributes to enhanced patient safety and a reduction in medical errors. Real-time patient monitoring systems, for example, provide continuous surveillance of vital signs, alerting medical staff to potential critical events promptly. Barcoding and RFID technologies minimize medication errors by verifying patient identity and medication accuracy before administration. Furthermore, computerized physician order entry (CPOE) systems reduce transcription errors and improve the clarity of medical orders, minimizing misinterpretations.
These systems, coupled with advanced analytics capable of identifying high-risk patients and predicting potential adverse events, contribute to a safer hospital environment. For instance, a study published in the Journal of the American Medical Informatics Association demonstrated a significant reduction in medication errors following the implementation of a CPOE system in a large hospital network.
Benefits of Telehealth and Remote Patient Monitoring
Telehealth and remote patient monitoring (RPM) expand access to care, particularly for patients in remote areas or those with mobility limitations. RPM utilizes wearable sensors and connected devices to collect physiological data, which is transmitted to healthcare providers for continuous monitoring. This allows for early detection of health deterioration, enabling timely intervention and preventing hospital readmissions. Telehealth consultations, conducted via video conferencing, provide convenient access to specialists, reducing the need for costly and time-consuming travel.
For example, RPM programs have shown effectiveness in managing chronic conditions like heart failure and diabetes, resulting in improved patient outcomes and reduced healthcare costs. Telehealth has also proven valuable in providing mental health support, offering patients a convenient and accessible alternative to in-person therapy.
Personalized Medicine Implementation
Smart hospitals are increasingly incorporating personalized medicine approaches, tailoring treatment plans to individual patient characteristics. Genomic sequencing and other advanced diagnostic tools provide detailed information about a patient’s genetic makeup, informing treatment decisions and predicting potential drug responses. This approach allows for the selection of the most effective therapies while minimizing adverse effects. For example, targeted cancer therapies are personalized based on a patient’s tumor genetic profile, leading to improved treatment outcomes.
Furthermore, the use of artificial intelligence (AI) and machine learning algorithms enables the analysis of vast datasets, identifying patterns and insights that can further refine personalized treatment strategies. The integration of these technologies leads to more effective and efficient healthcare delivery, improving patient outcomes and quality of life.
Impact of Digital Patient Records on Streamlining Healthcare Processes
Electronic health records (EHRs) have revolutionized healthcare processes, enabling seamless information sharing among healthcare providers. This reduces redundancies, improves care coordination, and minimizes the risk of medical errors associated with incomplete or inaccurate information. EHRs facilitate the efficient retrieval of patient medical history, allowing for informed decision-making and personalized treatment planning. Moreover, EHRs support the implementation of clinical decision support systems (CDSS), which provide clinicians with real-time guidance and alerts based on best practices and evidence-based guidelines.
This enhances the quality of care and reduces the likelihood of diagnostic and treatment errors. The ability to analyze large datasets within EHRs also enables population health management, allowing for proactive identification of at-risk individuals and the development of targeted preventative strategies.
Patient Journey Map in a Smart Hospital
The following describes a patient’s experience in a smart hospital, highlighting technological touchpoints:A patient, experiencing chest pain, arrives at the emergency room. Upon registration, biometric data (fingerprint or facial recognition) confirms their identity, expediting the process. Smart triage systems assess the patient’s condition, prioritizing their care based on urgency. Wearable sensors monitor vital signs continuously throughout their stay.
Diagnostic imaging is performed using advanced technologies such as AI-powered image analysis, providing faster and more accurate results. Physicians access the patient’s complete EHR, including past medical history and current test results, facilitating informed decision-making. Treatment is personalized based on genetic information and predictive analytics. Post-discharge, the patient receives remote monitoring through connected devices and telehealth consultations, ensuring continued care and support.
Throughout the entire process, the patient interacts with intuitive digital interfaces, providing a seamless and personalized experience.
Challenges and Considerations in Implementing Smart Hospital Technologies
The transition to smart hospitals, while promising significant improvements in patient care and operational efficiency, presents a complex array of challenges that require careful consideration and proactive mitigation strategies. These challenges span technical, ethical, economic, and legal domains, necessitating a holistic approach to implementation and ongoing management. Failure to address these challenges effectively could hinder the realization of the full potential of smart hospital technologies and potentially compromise patient safety and data security.
Potential Security Risks Associated with Storing and Transmitting Patient Data
The digitization of patient data inherent in smart hospital systems introduces significant security vulnerabilities. The interconnected nature of these systems creates numerous potential entry points for malicious actors seeking to access sensitive information. Risks include data breaches through unauthorized access, malware infections, and insider threats. The transmission of data, whether via internal networks or external connections, is also vulnerable to interception and compromise.
For example, a poorly secured Wi-Fi network could allow unauthorized access to patient records, while vulnerabilities in data encryption protocols could allow data to be decrypted and stolen. Furthermore, the sheer volume of data generated in a smart hospital increases the complexity of security management and the potential for human error.
Ethical Implications of Using AI in Healthcare Decision-Making
The increasing use of artificial intelligence (AI) in healthcare decision-making raises several ethical concerns. Bias in algorithms, stemming from the data used to train them, can lead to discriminatory outcomes, potentially exacerbating existing health disparities. For instance, an AI system trained primarily on data from a specific demographic group may perform poorly when applied to other groups. Furthermore, the lack of transparency in some AI algorithms makes it difficult to understand how decisions are made, raising concerns about accountability and the potential for errors to go undetected.
Questions also arise regarding patient autonomy and the potential for AI to override or influence clinical judgment without proper oversight. The responsibility for errors made by AI systems needs to be clearly defined.
Cost-Effectiveness of Implementing Smart Hospital Technologies
The implementation of smart hospital technologies represents a substantial financial investment. The initial costs of purchasing and installing new equipment, software, and infrastructure can be significant. Furthermore, ongoing maintenance, updates, and staff training add to the overall cost. The return on investment (ROI) can be difficult to quantify, as the benefits of improved efficiency and patient outcomes are not always easily measurable in monetary terms.
A thorough cost-benefit analysis is crucial before embarking on a smart hospital initiative, taking into account all potential costs and benefits, both tangible and intangible. For example, the cost of implementing a new electronic health record (EHR) system must be weighed against the potential savings from reduced administrative burden and improved patient care coordination.
Need for Robust Cybersecurity Measures to Protect Patient Data
Robust cybersecurity measures are paramount in protecting patient data within a smart hospital environment. This requires a multi-layered approach incorporating several key elements. Firstly, strong access control mechanisms, including multi-factor authentication and role-based access control, are essential to limit access to sensitive information. Regular security audits and penetration testing can identify vulnerabilities and weaknesses in the system. Data encryption, both in transit and at rest, is crucial to protect data from unauthorized access even if a breach occurs.
Furthermore, staff training on cybersecurity best practices is essential to prevent human error from becoming a security vulnerability. Incident response plans should be in place to manage and mitigate the impact of any security breaches. Investing in advanced threat detection systems and utilizing threat intelligence feeds can proactively identify and address potential security risks.
Comparison of Different Data Privacy Regulations and Their Impact on Smart Hospital Implementations
Various data privacy regulations, such as HIPAA in the United States, GDPR in Europe, and others around the world, significantly impact the implementation of smart hospital technologies. These regulations dictate how patient data can be collected, stored, processed, and shared. Compliance with these regulations requires significant investment in infrastructure, processes, and personnel. Differences between regulations can create challenges for organizations operating across multiple jurisdictions.
For example, the GDPR’s stringent requirements for data consent and data subject access requests may necessitate changes to data management practices in smart hospitals. Failure to comply with these regulations can result in substantial fines and reputational damage. Understanding and adhering to these regulations is critical for the responsible and ethical deployment of smart hospital technologies.
The Future of Smart Hospitals

The convergence of artificial intelligence, the Internet of Things (IoT), and big data analytics is poised to revolutionize healthcare delivery within smart hospitals. Future trends will focus on enhancing patient experiences, improving operational efficiency, and fostering a more proactive and preventative approach to healthcare. This will involve a deeper integration of various technologies, creating a truly interconnected and intelligent healthcare ecosystem.
Future Trends in Smart Hospital Technology
Predicting the precise trajectory of smart hospital technology is challenging, but several key trends are emerging. These include the increasing adoption of AI-powered diagnostic tools capable of analyzing medical images with greater speed and accuracy than human clinicians, leading to faster diagnoses and improved treatment plans. Robotic surgery will become more sophisticated, offering minimally invasive procedures with enhanced precision and reduced recovery times.
Furthermore, personalized medicine, driven by genomic data analysis and AI-powered predictive modeling, will tailor treatments to individual patient needs, optimizing outcomes and reducing adverse effects. The expansion of remote patient monitoring (RPM) systems, leveraging wearable sensors and IoT devices, will allow for continuous health data collection and proactive intervention, reducing hospital readmissions and improving patient outcomes. Finally, the development of advanced cybersecurity protocols will be crucial to safeguarding sensitive patient data within the increasingly interconnected smart hospital environment.
Blockchain Technology for Enhanced Data Security and Interoperability
Blockchain technology offers a promising solution to the challenges of data security and interoperability in healthcare. Its decentralized and immutable nature ensures the integrity and confidentiality of patient records, reducing the risk of data breaches and unauthorized access. By creating a secure, shared platform for healthcare data, blockchain can facilitate seamless information exchange between different healthcare providers, improving care coordination and reducing medical errors.
For example, a patient’s medical history, including allergies, medications, and test results, could be securely stored on a blockchain and accessed by authorized healthcare professionals across different institutions, ensuring consistent and informed care. This enhanced interoperability would streamline administrative processes and reduce redundant testing. The implementation of blockchain, however, requires careful consideration of regulatory compliance and the development of robust security protocols to prevent malicious attacks.
Innovative Applications of Virtual and Augmented Reality in Medical Training and Patient Care
Virtual reality (VR) and augmented reality (AR) are transforming medical training and patient care. In medical training, VR simulations provide immersive and realistic environments for practicing complex surgical procedures, diagnosing diseases, and managing medical emergencies, improving the skills and confidence of healthcare professionals. For instance, surgeons can practice intricate procedures in a risk-free virtual environment before performing them on real patients.
AR overlays digital information onto the real world, guiding surgeons during operations or assisting healthcare providers in locating veins for intravenous injections. In patient care, VR can be used for pain management, rehabilitation, and psychological therapy, offering engaging and effective treatment options. For example, VR can distract patients from pain during procedures or provide immersive experiences for physical therapy exercises.
AR can enhance patient understanding of their conditions by providing interactive 3D models of their anatomy or visualizing treatment plans.
Timeline of Key Milestones in Smart Hospital Technology Development
The development of smart hospital technology has been a gradual process, with key milestones occurring across several decades. A simplified timeline highlights significant advancements:
- 1970s-1980s: Early adoption of computerized physician order entry (CPOE) systems and hospital information systems (HIS).
- 1990s-2000s: Emergence of electronic health records (EHRs) and Picture Archiving and Communication Systems (PACS) for digital image storage and retrieval.
- 2010s: Rapid growth of the Internet of Things (IoT) and the integration of wearable sensors for remote patient monitoring (RPM).
- 2020s-Present: Increasing adoption of artificial intelligence (AI) and machine learning (ML) in diagnostics, treatment planning, and predictive analytics; exploration of blockchain technology for data security and interoperability; widespread use of virtual and augmented reality in training and patient care.
Integration of Smart Technologies for Efficient and Effective Healthcare Delivery
The integration of various smart technologies in hospitals promises to significantly enhance the efficiency and effectiveness of healthcare delivery. For example, the combination of AI-powered diagnostic tools, EHRs, and RPM systems can facilitate proactive patient management, enabling early detection of potential health issues and timely interventions. This integrated approach can lead to reduced hospital readmissions, shorter hospital stays, and improved patient outcomes.
Furthermore, robotic surgery, coupled with AR guidance, can improve surgical precision and reduce recovery times, leading to enhanced patient experiences. The use of blockchain for secure data sharing can streamline administrative processes and improve care coordination, reducing costs and improving efficiency. The overall effect is a more patient-centered, data-driven, and cost-effective healthcare system.
Case Studies of Successful Smart Hospital Implementations
The successful implementation of smart hospital technologies requires a multifaceted approach, encompassing technological integration, staff training, and a robust data management system. Examining specific case studies reveals the diverse strategies employed and the resulting improvements in patient care and operational efficiency. These examples highlight both the potential benefits and the challenges inherent in transforming traditional healthcare facilities into technologically advanced smart hospitals.
The Cleveland Clinic’s Smart Hospital Initiative
The Cleveland Clinic, a large, multi-specialty academic medical center in Ohio, USA, has undertaken a comprehensive smart hospital initiative.
- Hospital Size and Location: A large, integrated healthcare system with multiple hospitals and clinics across Northeast Ohio, USA.
- Type of Services Offered: Comprehensive range of medical services, including cardiac care, neurosurgery, oncology, and more.
The Clinic has leveraged various technologies, including advanced analytics to predict patient needs and optimize resource allocation, electronic health records (EHR) for seamless data sharing, and remote patient monitoring systems to enhance post-discharge care. The implementation involved significant investment in infrastructure and staff training. Outcomes include improved patient satisfaction scores, reduced hospital readmission rates, and enhanced operational efficiency through optimized resource allocation.
Challenges included data integration across various legacy systems and the need for ongoing staff training to adapt to new technologies. The Clinic’s phased approach, prioritizing high-impact areas first, mitigated risks and ensured a smoother transition.
Royal Papworth Hospital’s Digital Transformation
Royal Papworth Hospital, a specialist heart and lung hospital in Cambridge, UK, represents a successful case study in digital transformation.
- Hospital Size and Location: A medium-sized specialist hospital located in Cambridge, UK.
- Type of Services Offered: Specialized services focused on cardiology, respiratory medicine, and related surgical procedures.
Their approach involved implementing a comprehensive electronic patient record system, integrating various medical devices to create a connected care environment, and deploying telehealth technologies for remote patient monitoring. This resulted in improved clinical decision-making, enhanced patient safety through reduced medication errors, and streamlined administrative processes. Challenges included addressing concerns about data security and ensuring the interoperability of different systems.
The hospital’s commitment to staff training and engagement was crucial to the successful adoption of these new technologies.
Sheba Medical Center’s Smart Hospital Project
Sheba Medical Center, a large medical center in Tel Hashomer, Israel, has embarked on an ambitious smart hospital project.
- Hospital Size and Location: A large, tertiary care hospital located near Tel Aviv, Israel.
- Type of Services Offered: A comprehensive range of medical services, including advanced treatments and research.
Sheba has implemented a range of technologies including AI-powered diagnostic tools, robotic surgery systems, and predictive analytics for resource management. The outcomes include improved diagnostic accuracy, reduced surgical invasiveness, and optimized resource allocation. The challenges included the high initial investment required and the need for ongoing system maintenance and updates. Sheba’s strategic partnerships with technology providers and its commitment to continuous innovation have been key factors in its success.
The integration of technology in healthcare is not merely an incremental improvement; it represents a fundamental transformation of how medical services are delivered and experienced. Smart hospitals are poised to redefine patient care, fostering a more efficient, personalized, and safer environment. While challenges remain in areas such as data security and ethical considerations, the potential benefits of these technological advancements are undeniable.
Continued innovation and responsible implementation will pave the way for a future where technology empowers healthcare professionals to provide the highest quality of care, ultimately leading to healthier populations worldwide. The ongoing evolution of smart hospital technology necessitates a proactive and adaptive approach, balancing innovation with ethical considerations and robust security measures to ensure a future where technology enhances, rather than compromises, the quality of patient care.
FAQ Resource
What are the major cybersecurity threats facing smart hospitals?
Major threats include data breaches through ransomware attacks, unauthorized access to patient records, and vulnerabilities in connected medical devices.
How do smart hospitals address the issue of data privacy?
Smart hospitals utilize robust encryption, access control measures, and adherence to regulations like HIPAA (in the US) and GDPR (in Europe) to protect patient data privacy.
What is the role of human interaction in a smart hospital?
While technology plays a significant role, human interaction remains crucial for patient empathy, communication, and complex decision-making. Technology serves to augment, not replace, the human element.
What are the potential job displacement concerns with automation in smart hospitals?
While some tasks may be automated, new roles focused on technology management, data analysis, and specialized healthcare support are likely to emerge, requiring retraining and upskilling of the workforce.
How do smart hospitals manage the integration of various technologies from different vendors?
Effective integration requires careful planning, standardized interfaces, and robust interoperability protocols to ensure seamless data exchange between different systems.